Lao Birthwork
Nourishing natural birth wisdom in Laos
Lao Birthwork is a voluntary project that was inspired by having made several trips to Luang Prabang province in northern Laos between 2005 and 2015. During my visits there, and through Laos contacts and friends working in Maternal and Child Health, I witnessed which services and training had and hadn’t been made available by the government and some of the established NGOs. My interest really lay with wanting to understand more about the traditional systems of birth care and the ‘mortum yae’ – traditional birth attendants, and how they were supported. Where they exist, traditionally they come from a lineage of birth knowledge being passed from mother to daughter. Around 2005, I was fortunate to spend a little time with some ‘mortum yae’ in traditional villages. They hadn’t come from a lineage, but had some training as health workers for their village and then took on the role of attending births. This still happens sometimes, and sometimes it happens the other way around. Some mortum yae are trained as health workers.
Even though the mortum yae have been valued til recently, the acknowledgement and support of traditional birth attendants within their own communities is no longer on the agenda of international aid agencies, and therefore no longer on the agenda of poor governments who rely on the aid agencies to channel money for establishing health services. Their preference and priority is to channel money and resources in to establishing a number of small clinics in each district and training health staff to work there. Clinic staff have to deal with all manner of medical problems, and also provide women and babies with antenatal, birth and postnatal care.
The Laos government also supervises any excursions and trainings, so my dream of spending time with mortum yae in remote areas was, and is still is, not easily realized. When an invitation came to bring training to minimally trained and under-resourced ‘professional’ care providers, I graciously accepted. I then set about bringing together core team members – dear friends who were well experienced in hands on skills for complications, and also body-oriented skills for preventing and dealing with obstructions. Between the 4 of us we have experience in birth education, midwifery education, homebirth and hospital birth attendance, maternal and child health, bodywork, body-oriented birth skills and working with other cultures.
For the last 4 years, 2016-2020, our team has raised funds for the project. We have to provide financially for every aspect of the venture, other than a vehicle which is provided for us. Each participant receives an allowance to enable them to travel, eat and stay close to the training. We provide each participant with a bag of essential supplies – nail brush, nail scissors, disposable gloves, scourers, cotton twine, torch, fetoscope, lubricant, tape measure, notepad, pens etc. And we take much needed supplies to give out such as infant bag/masks, dolls for education, posters and hot water bottles for comfort. We also buy blankets, pillows, towels, vinyl mats, basins, batteries and other essentials.
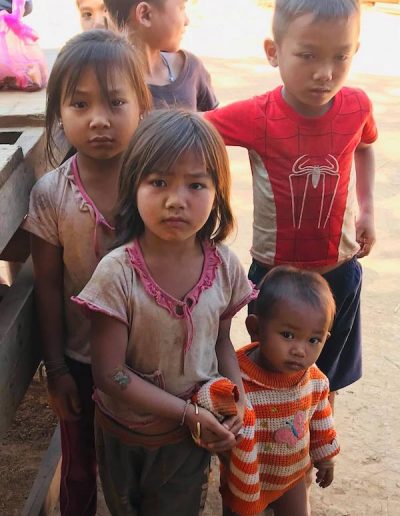
We teach in the remote district hospitals and health centres of Luang Prabang province, where the terrain is extremely mountainous, and roads and tracks to remote villages impassable in the wet season. Though the population in Laos is less than 8 million there are 53 known ethnicities – with one estimate of over 100 ethnicities. Cultural beliefs and world views differ greatly between groups. A large number of villages are so remote that they are largely unreachable and not registered with the government. Apart from trade with neighboring villages, they are self- sustaining in their subsistence lifestyle. Many ethnicities have a distrust of modern medicine, and the cultural norm for them is to birth at home.
Within some ethnic groups, restricted diets after birth can cause problems in the health of infants. Restricted diets may be based on poverty but also beliefs about the harm certain foods will do.
It is only in the last 2 decades that Laos has been in recovery from the fallout of the Vietnam war, followed closely by the disruptive change to Communist government in 1975. During the Vietnam war, massive, widespread bombing occurred in the north with US army planes indiscriminately dropping leftover bombs into Laos territory after their bombing sorties in the mountains of Vietnam. Consequently, Laos, who wasn’t part of the Vietnam war, is considered to be the most bombed country per capita in history, and mountain communities are still living and dealing with the threat and deadly legacy of UXO – unexploded ordinances.
There was also great fracturing of Hmong mountain communities during The American Secret War against communist rule when the CIA, on the side of the royalists, enlisted the Hmong to fight for their interests. The fiercely independent Hmong had innate warrior capabilities and didn’t want political change either, just as most independent mountain people around the world feel about bending to political will. After the war, they were persecuted by their own government, and inadequately supported by the departed Americans. Many became refugees, with some still in the process of being repatriated.
And in post war and economically poor Laos, some of the making amends to such devastation came in the form of global ideals and global aid to improve the relatively high maternal and infant mortality rates so common in impoverished countries. The focus has been on establishing small health clinics with trained staff who provide maternity services and encourage all mothers to access them. Seeking to bring everyone into this clinical orbit is a huge task, if not an impossible one that is trying to be accomplished through the constantly shifting sands of international aid organization targets, assessments, ideals and priorities.
The style and content of our trainings tends to be somewhere between where the clinical model and training ends, and the traditional model begins. We bring our 3 days of ‘hands-on skills for birth’ training to a central gathering of midwives, doctors, nurses and health workers (who are living in some of the most remote villages). This is appreciated as there is very little training that actually goes out to the districts and brings all the health staff together, so that they are connecting and learning together.
The foundation of our training is Birthwork’s ‘The 3 Kindnesses’
This is presented as a logical imperative to better outcomes.
- Be kind to each other. Share information at every opportunity to those in your community. When people are educated about birth and their bodies, woman and babies and communities are healthier.
- Be kind to the mother. Her job is the most important job in the world. It is more important than your job. Treat every woman as though she were a dear sister to you, even if you have judgments towards her. When you are kind with your touch, your words and your actions, the mother will relax and she will birth more easily. whatever happens, the mother and her family will remember the kindness.
- Be kind to yourself. Be prepared for any situation. Ask for help if you need it. Have your backup plans and transport plans in place. Rest well, eat well, sleep well.
Poverty and challenging access to medical care remain the biggest health threats to women and babies and communities in general. We heard stories and sometimes saw for ourselves women who had walked for 6 hours to reach help at a clinic in pregnancy or during or after birth. And then were transferred by boat or by tractor or ambulance on dangerous roads for another 4 hours to a small district hospital. Once the promise of medical care is available to even the remotest communities, they will come, but usually when all else has failed. Birth in the clinics and district hospitals is still estimated to be at about 30%. The rest are homebirths.
Transport when it is available and necessary, is often costly and can further impoverish families that live at subsistence level. Sometimes, especially during the wet season, transport is impossible. Women in Laos generally birth quickly. A first-time mother is expected to deliver in 4 hours. Subsequent births are expected to be shorter. Unless truly needed, transporting in labour on bumpy dangerous roads by scooter, tak tak (tractor type of trailer), or even by car, can be a danger in itself.
The ideal of having all women access antenatal care and birth at the clinics is fraught with so many logistical challenges. At the most, regular antenatal care can help identify some predictable problems and ensure the mother is referred for more complex medical care, but it won’t identify the unpredictable incidences of haemorrhage, premature birth, babies who need resuscitation, babies who get stuck, and surprise breech and multiple births.
This is where we come in. Our aim with the training is to replenish confidence and morale and skills. And to also plant and nurture seeds that will grow natural birthing knowledge and wisdom that can easily flourish in any environment, conditions and circumstance, and within any culture.
At the last training we did, in a very remote district, they had never had anyone come to do any kind of refresher training around birth. None of the 30 participants – who were health workers, midwives and nurses had received any training in newborn resuscitation, shoulder dystocia or breech birth. They were working in isolated clinics, under difficult conditions with very limited resources, and responsible for a number of outlying villages in their area.
We spend time visiting some of those outreach clinics, refreshing emergency skills for staff, and inviting village women along too for discussion and demonstrations. We show the clinic staff how they can accommodate women who prefer to birth in more traditional positions other than on their backs. We also encourage community information days, so that women and men can come together and ask questions and share information about all aspects of birth. We’ve developed posters and a pictorial booklet to illustrate the aspects of what we teach.
We are learning so much about this gentle culture, and about the politics of international development. We are learning more about the obscene imbalance of wealth, power and resources in a world that spends inordinate amounts of money on weapons and a relatively miniscule amount on ensuring the wellbeing of mothers and babies. And we are reminded about how birth is still largely and naturally successful even without the medical care for emergencies that we so easily take for granted in our wealthy culture. And how it can be even more successful when knowledge is freely shared. And we are witnessing how women still wish to have choice, all things considered, around where and with whom they will birth.
And more…
When we first began coming to Laos to offer what we felt was missing, and what we knew we could teach with integrity and authenticity, it still felt like such a drop in the vast ocean of needs. We are at the complex interface of the implementation of global ideals of maternal and child health care meeting birth traditional and subsistence lifestyles and worldviews.
But to date we have twice connected with around 120 birthworkers from 4 districts in the province. They are health workers, nurses, midwives, medical assistants, doctors, senior midwifery trainers at Luang Provincial hospital and Swiss Red Cross, and the Maternal and Child Health Head from the Provincial Health Department. They have also connected with each other and learned valuable birth basics together. The drops are becoming little rivulets, and it feels good.
Luang Prabang province has 12 districts.
Each district has a small district hospital and maternity unit.
Each district also has a number of ‘sok sala’ or health clinics that are situated within a village but also serve as a medical hub for a number of surrounding villages. The most remote ‘sok sala’ are known as outreach. And beyond outreach are some villages where Health Care and Home Care workers care for villagers in their traditional home. They may have had up to 6 months training and deal with any medical problems within the village.
Medical assistants have 3 years training and qualify via an English exam. They do all kinds of tasks at the district hospital. It takes another 6 years study to become a doctor.
Midwives have 2 Years training either in Laos, Vietnam, or Thailand
Traditional birth attendants still exist in some villages, but we have no access to them with our project. The PHD, and the big aid agencies do not support TBA’s with training in this province.
Jenny Blyth
Please find below a day by day description of our last 2 trips by Steffi . Steffi posted on Facebook every day to keep our wonderful supporters informed of exactly what we were doing and where we were.
Also find attached some reports drafted by Dr. Katharine McKinnon, a social geographer and academic from La Trobe university who accompanied us on our last 2 trips to evaluate our pedagogical approach. They make for a very interesting read and a deeper insight into many more aspects of the interface that exists between the traditional and medical approaches to birth.
29th Jan 2019 Facebook Post by Stef
Yesterday we began our current training at the Phon Thong District Hospital.
Phou Thong has a population of 20,000 people. The district has 5 health centres which service over 42 registered villiages. There is also an unknown number unregistered villages, comprised of ethnic minority communities who live a independent subsistence lifestyle without involvement, regulation or support from government organisations.
Due to the isolation of many of the registered villages, Phon Thong district offers a mobile midwifery & medical clinic that travels through profoundly mountainous terrain every three months.
At the beginning of training we received a generous opening ceremony conducted by a local health offical. There were many words of thanksgiving & well wishes for our families on account of our willingness to travel so far & to be of support to their isolated community.
There are 30 Midwives, Doctors & Health Workers who are joining us for the training, 15 of whom had travelled many hours from even more remote villages in order to be here.
Once again throughout the training we are continually emphasising the foundation of kindness which is at the heart of all our teachings; nurturing trust & safety with the mothers & families in our care.
We explored kindness & generosity in the sharing of knowledge, kindness compassion & commitment to the mothers & babies in our care & kindness, compassion & commitment to self care, wellbeing, resourcefulness & organisation as care giver.
We explored supporting the third stage of labour; how to support a mother’s wellbeing & how to respond in the instance of a haemorrhage or a retained placenta; proposing that warmth, communication, safety, skin to skin contact with the baby & breastfeeding are important ways to support the prevention & management of pph.
A midwife from a remote health centre shared the story of a mother who experienced a retained placenta & bleeding after a homebirth in a remote village. The birth occurred during the rainy season & the mother was required to travel 7 hours by night, plus 2 separate boat trips & a 3rd vehicle transfer to Luang Prabang Hospital (3 hours) to eventually receive the required surgical assistance that the she needed.
A young male health worker shared the story of a mother who had suffered 2 or three days of significant bleeding after birthing in a mountainous village. The mother’s placenta was retained but with his support & assistance the placenta was born & the mother though in a compromised condition was able to recover.
In Laos active management of the third stage of labour & the use of syntocinon is routine although in some villages traditional medicine is also still used by the traditional birth attendants.
Claire explored the main reasons for pph being Tone, Tissue, Thrombin & Tears & taught her catchy 10 step approach to managing postpartum emergency. She has also created a series of actions to accompany each step of emergency care which definitely seems to provide an effective means to absorb the important information she is imparting.
After lunch we worked our way through Newborn Resuscitation & discovered that
numerous health centres did not have any baby resuscitation equipment. If anyone has access to quantities of newborn bags & masks please let us know as we have realised that they are an essential requirement in remote Laos. We hope to provide them as donations during our next trip.
Once again we introduced delayed cord clamping & explained that while it is not current practice in Laos it is the recommendation of WHO; a baby only has approximately 250 mls of blood & around 1/3 of its blood supply still remains in the cord & placenta at the time of birth. At least 5 mins is needed for the placenta to cease pulsing & for cord to begin to drain. This information was all new learning to the participants in our training.
Claire once again went through another series of clear steps & actions and provided an opportunity of participants to practice with either bags and masks. The participants whose centres did not have bags and masks were asked to practice with a pinnard as an alternative tool.
3 pregnant mothers had travelled to the hospital specially to meet with us so while Claire & Jen continued with teaching Newborn Resuscitation & techniques to support Shoulder Dystocia. Katharine and I (Steffi) spent a couple of hours with the pregnant women, hearing their stories & concerns.
2 of the women were pregnant with their first babies & both lived locally, in close proximity to the hospital while the other had travelled all day (over 5 hours) by motor bike to reach the hospital.
She had birthed 5 babies but only 2 were still living. The 3 babies she had lost had only lived for a day. 2 of her babies were born preterm & the 3rd while born at term was very weak & experiences some kind of respiratory compromise.
The mother’s two living children had both been born at the hospital while the three that had passed away had been born at home.
Although her baby’s deaths & preterm births were most likely due to malnutrition & lifestyle or any number of other potential factors in the realms of blood compatibility or infection & not to the fact that they were born at home, the mother was determined to reach the hospital for this baby’s birth. The likelihood of this was slim as she had over 5 hours of motorbike travel for a 5th labour.
Staying at home in the care of loving relatives felt like the safest option but we found it hard to know how to best advise her as her wish to get to hospital was understandable considering the tragic losses that she has know this far. We also discussed other options such as the possibilities of staying with relatives in advance of both who lived close to a health centre. Knowing when to do this & how to manage her other children & the responsibilities of her daily subsistence life would not be easy circumstances to negotiate.
There was no easy solution we could offer to this lovely & stoic mother. I felt a sense of helplessness & concern for the potential of imparting information that would merely confuse & overwhelm her further or appear patronising & pointless in the scope of the profoundly challenging circumstances she lived within.
She lived a hard-working, farming life & with the support of her midwife was learning to take better care of herself and her nutrition during this pregnancy.
We spoke about the essential importance of good nutrition, adequate protein, fresh, green leafy vegetables & good hydration.
While she assured us that her farm provided access to good food it was had to ascertain the quantities of which she was eating & whether as the mother of the family she may be required to serve herself last in the chain of family members as is the case in many ethnic minorities.
We also spoke about the importance of rest & avoiding over excursion. One of the other mothers expressed that there was a belief that taking a rest was ‘not a good or safe practice for a pregnant woman.’
We went through some simple bodywork & spoke about how family members could assist her to rest and relax.
It felt like a simple offering without the shimmer of a sure solution but at the very least some kindness & care had been offered which I pray will be of some service.
I have found it hard to put this woman’s story down & have been ruminating upon all the additional things I could have offered & explored. I regret not giving guidance around the prospect of supporting a safe birth whilst en route to hospital or made enquires around breastfeeding and the importance of colostrum as some ethnic groups choose not to give it to their babies.
Thankfully we can speak further to the mother’s midwife & to help ensure that her and her husband receive the information that they need although as she is already 7 months pregnant it is hard to know whether they will see her again before she has her baby in her arms.
One of the other mothers had concerns about her baby’s positioning & was fearful about the risk of a surgical birth which would require a many hours long transfer.
We spoke about what she could do to support optimal positioning & went through some simple bodywork techniques. We also went through the benefit of birth in upright position & assured her that over the coming days we will be providing the local midwifes & doctors with new techniques that they will be able to use to support her should her baby find itself in a challenging position.
We gifted the women with Days for Girls Postnatal Kits & encouraged them to take what they needed for themselves, their babies and families from our big case of donated clothes.
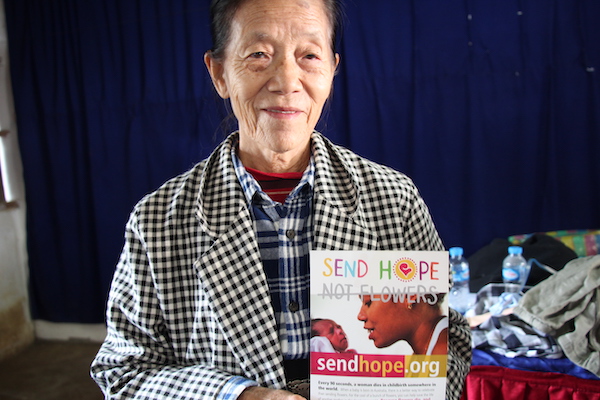
We continue to feel so grateful for all the donations of funds, supplies & resources that we have been given in advance of this trip & especially grateful for the Menstrual Health Kit donations from Days For Girls & the amazing primary funding we have received from Send Hope Not Flowers who have made this trip possible.
30th Jan 2019 Facebook Post by Stef
Our second day at Phonthong began with an exploration of breech birth.
Claire beautifully explained that most breech babies, when undisturbed will simply flop out & that the best position for the mother is to be on her hands & knees or in an upright, squatting, kneeling or standing position & that for a breech birth the safest approach is to keep your hands off!
She then went through the steps and actions to support a complex breech in the instance of a baby getting stuck. The midwives, doctors & health workers were again able to experience playful enactments to practice the different techniques that were taught. Once more it was so heartwarming to see all of our participants joining in so enthusiastically & again the male doctors were gorgeous to observe as they gave themselves so wholeheartedly to their breech birthing & baby catching practice.
The afternoon was spent exploring pelvic dynamics, the hormones of birth, dynamic birthing positions & simple bodywork to support space making, comfort & relaxation & turning babies in tricky positions.
During Katharine’s time of class evaluation & enquiry participants claimed that everything that we had covered was new learning to them; the emergency skills, the concept of delayed cord clamping, the prospect of positional changes & bodywork & the influence of kindness & compassion upon the wellbeing of mothers.
In this remote part of Laos there are few opportunities for deepening education. Once one’s initial & often quite limited training is complete it seems that you are left to your own resources with little or no opportunity to deepen or broaden your skill base.
Phonthong district is the most remote of all the areas that we have taught in through our 3 Laos Birthwork Trips.
There are many unique challenges that occur due to the level of isolation, lack of education, lack of resources & the extreme conditions of the rainy season.
Particular challenges pertaining to language barriers are also very common between the different ethnic groups that exist in this area.
Laos has a population of over 6.49 million people. While 54% of the population is comprised of the Lao Loum (or the low land Lao) who speak the predominant Lao language the remaining 46% are broken into 4 main ethnic minority groups. In truth it is not really known how many groups exist though it is proposed that there could be as many as 100 different ethnolinguistic groups throughout the country.
This region has one of the highest densities of ethnic minority groups which means that language & cultural barriers exist as common hurdles in health care.
For the first time in our trainings the participants opened up about different traditional practices that are used around birth. We were shown a couple of massage techniques, one for labour & one for after birth & were told about the heating of stones that are wrapped in leaf parcels of a specific herb & then wrapped in cloth bundles and used as a compress over a new mother’s body & also about a practice of ‘mother roasting’ where a new mother will rest over a bed of hot coals or stones.
It was beautiful to hear these examples of traditional practices & encouraging to know that they still live on despite the greater medicalisation of birth.
This morning a pregnant mother arrived at the hospital with symptoms of pre -eclampsia & polyhydramnois.
She initially walked 2 hours to reach her local health centre & was referred to the district hospital once an irregular heartbeat was detected in her baby & her concerning symptoms where seen. She then walked 4 hours to reach the hospital & upon arriving her baby’s heartbeat was found to be very high.
She was transferred a further 4 hours by ambulance to another hospital with better resources but so sadly her baby passed away on the way to the hospital.
The Maternal Child Health Official who is involved in hosting our trip shared the news of the baby’s passing.
We are all feeling deeply for her & for the little baby, the mother & family. The complexities involved in effecting change in these beautiful yet isolated & under resourced circumstances are innumerable. We finished our day with heavy hearts.
31st Jan 2019 Facebook Post by Stef
Our final day of training at Phonthong District Hospital began with Jen’s introduction to the value of keeping palpation skills alive. Using Claire & a baby doll as models she went through some simple steps of helping make sense of how to feel a baby in different positions.
She then used a pinnard to demonstrate the simple yet invaluable wisdom of how to make sense of where a baby is lying based on the combination of where the heartbeat is heard most strongly, & palpating, & shared some specific bodywork techniques for turning babies in potentially challenging positions.
After a lot of confusion due to what was lost in translation, we were able to clarify that vaginal examinations in labour were no longer routine but that they were routinely given in late pregnancy to screen for infection. We were also able to clarify that mothers were consistently afraid of vaginal examinations, were afraid that they would hurt & concerned for their privacy.
Claire and I performed our midwife/ mother role play demonstrating two different approaches to giving a vaginal examination one emphasising gentle, patient & respectful communication, hygiene & touch & the other a rough, impatient, unhygienic & disrespectful approach.
We discussed simple ways that vaginal examinations can be respectfully & more gently given & emphasised the importance of kind, gentle & patient communication & continuing to steer away from their routine use during birth.
We finished the day with Katherine gathering feedback & doing her best to evaluate the appreciation, value & relevance of our training.
We received many words of gratitude and were further affirmed for the value & hopeful benefit of the teaching, specifically the emergency responses, positioning & bodywork techniques & appreciation for our willingness to travel to the district. Our training has been the only group training that has come to the doctors, midwives & health workers in this area.
Ultimately it is so hard to know whether or not we have truly offered something of value & how our offerings will translate in practice. We truly hope that even if it’s just in the smallest of ways we have provided something to improve outcomes for mothers & babies in these isolated & challenging circumstances & in some way helped to lift the morale & offered something of nourishment to these courageous midwives, doctors & health in support of their incredible work in their remote reaches of the world.
We completed the training handing out further supplies, Days for Girls Menstrual Health Kits & clothing, giving extra quantities to the midwives & health workers from the most remote villages.
1st Feb 2019 Facebook Post by Stef
Prior to leaving Phonthong District we travelled further west, toward the Vietnamese boarder to the village of Bandon, a beautiful & humble riverside township of thatched huts, a sweet little school, a couple of bamboo framed shops, racks of drying broom grass & a little health centre
The Health Centre’s nurse & midwife, both of whom had been present at our training shared further stories of the conditions & circumstances that they work in while showing us around their very clean but profoundly under resourced health centre.
They had no resuscitation equipment, no sheets, no blankets, no wash basins, no curtains, no power for extended times during the wet season & no emergency transport other than a raft to transport themselves out to the 5 other villages some of which span over a significant distance of remote & hard to access country. They had no means to transfer a birthing mother or other person in need when the river was high.
The young nurse & midwife work 7 days a week & are on call 24 hours a day & rarely receive a day off. We gave them all our remaining supplies – an infant resuscitation kit & a collection of Days for Girls Menstrual Health Kits, and a collection of clothing. On our next trip we intend to bring a more extensive collection of basic supplies to help better equip their centre.
En route to the next health centre in the village of Kewchilla we arrived at an accident where a mother, father, a small child & a baby, all travelling by motorbike had collided with another bike.
The mother has a small injury to her head & the father to his hand but amazingly the children were fine. The incident further illustrated the danger of these precarious roads & the tenuous nature of travelling through these breathtaking mountains particularly in a medical emergency.
Unlike the basic but beautiful village of Bandon which is set in a green & fertile river valley the village of Kewchilla is perched high on a dry & dusty mountain roadside. The land is arid & sparse & the quality of life felt harsh.
The Kewchilla health centre was similarly greatly lacking in resources but also cloaked in the thick layer of dust & a comparative sense of depravation that the township felt blanketed in. The young nurse & midwife who worked there had not yet finished their training & were therefore required to work as volunteers for an unknown period, surviving only on the limited support they received from their families.
Visiting these two health centres was a further confronting insight into the reality that the midwives & health workers we have been training live & work within.
On the whole there is no simple solution as to how to improve the quality of health or midwifery care in circumstances such as these. It was challenging & disturbing to step into such spaces, to hear the stories of tragedy that we were told & experience the breadth of complexities at hand.
We all found some comfort to see that one of Jen’s posters from our previous trip & the emergency response steps for PPH, Shoulder Dystocia & Newborn Resuscitation from this week’s training were stuck on the walls of each health centre ready to be used as reference points in the instance of need.
If you would like to contribute to our next Laos Birthwork Trip which will specifically support these two health centres & others like them & provide follow up training to the midwives, doctors health workers in this region & others you can do so on our go fund me page.
https://www.gofundme.com/34×46-lao-birthwork
Sharing our heartfelt thanks to everyone who has made this Laos Birthwork trip possible,
To everyone who has so generously donated funds to our go fund me campaign or other fundraising.
To The Laos Midwives Fund, Prem Williams & Jethro Williams of Sacred Earth Music, Jennie de Varga of
Universal Reiki & to Send Hope Not Flowers & Emma Macdonald for our primary & profoundly generous funding.
Heartfelt thank to Michelle Gates & Days for Girls Ferntree Gully, Camberwell, Harvey Bay & Maroochydore, to all your devoted volunteers & to Carolyn Mandersloot & Indiana Hehir
helping with transportation – your 100s of gorgeous menstrual health kits have travelled far & wide around Northern Laos!
Many thanks to Katharine Islay McKinnon & Latrobe University Melbourne, your lovely companionship, translation, knowledge of Laos culture, your evaluation & feedback upon our training was all so much appreciated.
And loving gratitude to our translator, Phonsavan,
Piyanat Yamavirun, Meemee, Buakeao, Sengchan,
Dr Vannaly & all other staff at The Laos Swiss Red Cross & The Provincial Health Department, your support, welcoming & hosting is so much appreciated.
So many thanks to everyone who has followed our journey, offered words of encouragement & shared in both the beauty & inspiration & the confrontation & sadness of what this adventure has held.
And the dearest thanks to our beloved families, communities & colleagues who have held the hearth in our time away from home – we can’t wait to see you!!
With love,
Jen, Claire & Steffi
January 2020 Facebook Posts by Stef
Back in beautiful Luang Prabang & after a big day of shopping at the local markets, we all are set with loads of supplies, to head north, on the windy, windy road to the district of Phonthong, towards the Vietnamese border.
This year we are bringing Days for Girls Menstrual Health Kits, pinnards & infant resuscitation masks, hot water bottles, clothes for mothers & babies, wash basins, towels, soap & scrubbing brushes, mats & mattress, sheets, blankets & curtains. These will be distributed among the midwives, doctors & health workers at our coming Birthwork trainings & also travel with us to some of the more remote & under resourced health centres that we will visit over the weeks to come.
Once again, this trip would not be possible without the support of our loving families & the amazing support & funding of Send Hope Not Flowers for which we are so grateful ❤ ️
At the end of a positive first day of Birthwork Training in Phonthong, Northern Laos….
With the majority of the 28 Midwifes, Nurses, Health Workers & Doctors present at last year’s trainings the focus of this visit is largely to follow up on last year’s teachings; how well they have been integrated, their relevance in practice, to gather stories of circumstances where challenges have been encountered, to hear how they were managed & whether our teachings have been of support.
Today we once again emphasised was ‘The 3 Kindnesses’ & their foundation at the heart of all we teach.
In Lao ‘Jai Dee’ is to ‘be kind’, to ‘be compassionate’.
In our teachings we are continually emphasizing the importance of being kind, respectful & generous with the knowledge that we hold as a care-providers.
Being kind to the mothers in our care through our words, touch & actions – during pregnancy, birth & postpartum. Remembering always that the mother’s job is more important than ours as care providers, she is our priority & we must treat her like the dearest sister no matter who she is. When a mother receives kindness, she has more reason to trust & relax & a relaxed body works best during birth. A mother will always remember the kindness she has received during birth.
And finally, being kind to yourself as a care provider; eat, rest, keep up to date with knowledge, have back up on hand if needed & being sure that our equipment is functional & ready if in need.
The larger part of the day recapped emergency skills for use in the instance of Postpartum Haemorrhage
( the most common cause of maternal death in Lao), Infant Resuscitation, Shoulder Dystocia & complex Breech Birth.
Yesterday’s training recapped the value of the pinnard & and attempted to address the glorification of the Doppler & other forms of ultrasound as the supposedly superior technology for assessing a baby’s wellbeing.
Many hospitals & health centres throughout remote Laos have been given Dopplers or bedside ultrasound machines & become quickly dependent on their use & convenience. With electricity & replacement batteries being unreliable & maintenance far from hand being in possession of ultrasound technology does not necessarily mean it is usable & even if it is there are so many reasons why dependence on the technology is questionable & concerning.
As is the case everywhere the value of the pinnard has been forgotten. We attempted to convey how its non-invasive impact, its assistance with confirming a baby’s position & its lack of dependence on electricity or maintenance are all qualities to celebrate.
Using both the example locating the baby’s heart rate with the pinnard & palpation skills Jen taught a beautiful passage on identifying baby positioning in pregnancy & in birth & the many reasons for keeping these hands-on skills alive & practiced.
We received some beautiful feedback around how different & appreciated our teaching style has been & how much easier it is to absorb & understand the information that we are relaying due to the experiential, fun & embodied nature of the activities we offer.
As has been the case in all our trainings we have got everyone out their desks & onto the floor, laying out the colourful woven mats that are common in most Lao homes & away from the rote style teachings that their westernised trainings thus far have emphasised.
It’s amazing how instantly the atmosphere softens, warms & relaxes from this simple change.
We followed up on pelvic anatomy & dynamics & how trust, safely, breath & positioning can influence relaxation in the mother & in turn make way for greater pelvic mobility & opening.
In a medicalised birth culture where birthing on one’s back with one’s leg in stirrups has been taught & practiced as the best position for birth it was so heartening to hear that since last year’s training several Midwives had been letting women know that they have the freedom to move freely during labour & choose positions most suited to their comfort at the time of birth.
There were some beautiful examples of midwives, in response to last year’s training inviting the assistance of family members to support birthing mothers in up right, squatting, kneeling, hanging & forward leaning positions as they would have used traditionally until the relatively recent arrival of western obstetric influence.
As always, the highlight of our day was practicing catching babies in different positions & practicing bodywork techniques to assist in babies positioning & a mother’s ease & relaxation during birth.
After several questions & confusion around safety in the third stage of labour we explored delayed cord clapping; the reasons, WHO recommendations & the comparisons of blood findings at 6 months between babies who have had delayed cord camping & those that have not.
Using an empty & a 1/3 full bottle of water Claire demonstrated the percentage of a baby’s vital blood supply that a baby is deprived of when the cord is cut prior to it stopping pulsing.
We also recapped the importance of compassion, kindness, clear communication & the utmost of respect when vaginal examinations are required. The Laos are very shy & private people & care providers & mothers alike can feel very afraid & uncomfortable about vaginal exams. Once again, we used our humorous & exaggerated role play to demonstrate ‘how’ & ‘how not’ to give a vaginal exam.
Our final day of training in Phonthong explored warning signs & complex circumstances in pregnancy, birth & postpartum & gave us a chance to trial Jen’s emergency response game which was received really well & and as hoped proved a really fun way to revise emergency skills.
Once again, we are fortunate to be sharing our trip with Katherine, a social anthropologist from Latrobe University in Melbourne. Katharine is here to document & evaluate our trainings as a part of an academic exploration & evaluation of birthing needs in Laos & the value & relevance of our trainings.
Her language & cultural insight are so wonderful to have on hand & through her facilitation a more thorough feedback & evaluation we are gathering a greater insight into the experience & impact of our trainings which has been really encouraging & affirming.
We completed our training handing out our bundles of donations – neonatal resuscitations kits, pinnards, disposable gloves, scrubbing brushes, floor mats, wash basins, soap, towels, blankets, baby & women’s clothing & Days for Girls Menstrual Health Kits all of which were received gratefully.
Many of the Midwives, Nurses, Doctors & Health Workers have come from remote & under resourced health centres where some of the most basic supplies are not present.
The offerings we have given were humble in comparison to the couple of requests for Doppler’s or humidity cribs that we received but having seen what we have thus far we are confident that our bundles will be of value.
An adventurous day in Northern Laos. Traveling on the windiest of roads, with terrible travel sickness we ventured further north of Phonthong, very close to the Vietnamese border & into beautiful, picturesque countryside. We spent the day visiting remote health centres, delivering donated supplies & Days for Girls Menstrual Health Kits & visiting traditional weaving villages in search of handwoven fabrics that we can use as fajas & rebozos in our work back home.
Traveling south west toward Lao’s Capital Vientiane we are now at the mountainous town of Phoukhone for this week’s training.
While setting up the space I was enthusiastically approached by a beautiful Hmong Doctor who we had met at last year’s training.
Despite the absence of Phonsvan, our translator & our complete lack of shared language he was determined to share with me what I soon gathered were many examples of how our training had been put to use over the past year.
He used gestures & enacted scenes to relay his experiences; squatting down on the ground & forward leaning over a table, to demonstrate a mother birthing in different positions, wrapping string around a water bottle & cradling the bottle in his arms with the string stretching down between his legs to depict delayed cord cramping & numerous actions related to pph management & shoulder dystocia.
When Phonsvan was present to translate he explained in greater detail how much he had learnt from our last visit & how useful this had been.
Even with the support of translators there is often so much that gets lost in translation leaving us uncertain of the extent to which our teachings have been received.
The Hmong Doctor’s passionate sharing & the many different circumstances he relayed was really affirming for us to hear.
Our first day of training went well & focused on emergency care, complex breech birth, shoulder dystocia & kindness.
Once again Jenny has devoted days of her precious time further refining our amazing handbook & creating a fantastic series of clear & succinct laminated handouts all accurately translated in Laos & beautifully illustrated & ready to mount in clinics walls to have on hand for guidance & clarification in emergency situations.
These booklets & handouts are possible to translate into any language. I am so excited that these resources are available & have no doubt that they will provide clear & lifesaving guidance in situations of need the world round.
Exploring catching babies in varied positions, pelvic dynamics, the baby’s decent through the pelvis, bodywork & rebozo, respectful vaginal examinations, palpation, the use of the pinnard, identifying baby’s position, cord entanglement & delayed cord clamping in Phoukhone, Northern Laos.
Affirmation of the value of our training flooded in with many stories of encouraging a mother to find positions of her choice other than birthing on her back & examples of delayed cord clamping which have developed since our visit last year.
Even the most remote health centres have been furnished with narrow obstetric beds & birthing on one’s back, with legs in stirrups followed by immediate cord clamping & cutting is routine practice.
It wonderful is so to hear that these practices are starting to change.
Sharing rebozo & other practices in support of pelvic mobility, comfort & baby positioning at our final day of training in Phoukhone, Northern Laos.
Our final birthwork adventure took us further into the mountains from Phoukhone & down to the river valley village of Banjim to visit 3 of the Midwives who had been present at our training.
With a health centre possessing only the most basic of facilities & a tiny birthing room with yet another archaic birthing bed at its centre we attempted to offer some inspiration around how the bed & general space could be used more creativity.
These courageous women care for mothers from villages that span over a 4 hour radius from their health centre.
They support woman who birth in the health centre but also travel by motor bike on rough dirt tracks to attend births at the homes of distant village women up to four hours away.
We were told they require a member of the military to accompany them on all of their visits which we assume is due to the social unrest & instance of rebel attacks which have been common in this area.
We offered the last of our Days for Girls Menstrual Health Kits, mothers & children’s clothes & general supplies to both the Midwives & their clinic & to some of the village family’s who we were taken to visit.
I had the privilege of tentatively stepping into the home of a beautiful mother who had birthed only a day before our visit to gift her with clothing & postpartum pads. I was able to sit for short time & observe her traditional postpartum practices of fireside warming, soup & tea drinking which felt very precious to witness.
We thank you all for your support & for sharing in our adventures!
We also give a wholehearted thank you to the amazing Send Hope Not Flowers who have funded our trip once again & enabled all our teachings, travels & gifting of supplies & resources to be possible.
Send Hope Not Flowers aims to help mothers & babies survive childbirth in the developing world.
They do this in numerous ways such as funding doctors and midwives to train local health workforces, purchasing obstetric equipment and basic supplies, delivering baby packs and helping mother’s access safe birth support.
They provide funding to partner organisations working on the ground in developing countries, on projects that are long-term, sustainable and empowering for women.
Send Hope is a small Australia based charity & are a wonderful, ethical & inspiring charity to consider donating to.